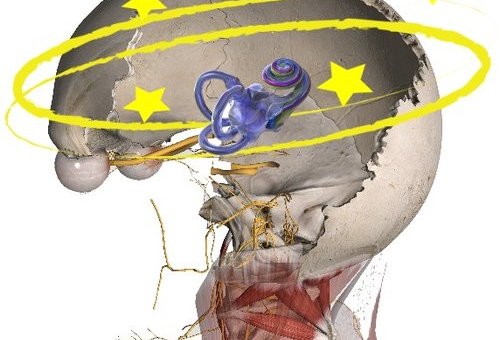
Vertigo is a sense of movement or rotation of the patient’s own or an external object.
When most people think vertigo, the most common diagnosis is benign paroxysmal positional vertigo (BPPV). This is long for BPPV and the same condition as when people think of crystals being out of place.
Most patients with BPPV report vertigo-like episodes when lying down, extending their head or neck, sitting up from a supine position, and bending over.
Another type of vertigo is nautical vertigo.
Nautical vertigo is defined as a sensory illusion reminding of movements experienced on board a ship in waves. It is not nearly as common and quite frankly, very limited information is out on this type of vertigo.
With that said, many patients may experience nautical vertigo instead of the typical symptoms of BPPV even though BPPV is much more prevalent.

In fact, an observational study in 2013 found nautical vertigo and dizziness are more common than rotatory vertigo in patients with chronic BPPV.
This could be due to individuals who suffer from vertigo can also have neck pain, headache, widespread pain, fatigue, visual disturbances, cognitive dysfunctions, nausea, and tinnitus. The combination of several symptoms, especially if chronic, can present differently.
The treatment for this type of vertigo does not always respond favorably to canalith repositioning procedures. Nautical vertigo will need more than cervical therapy too.
Individuals will most likely need more vestibular rehabilitation, sensorimotor training and cervical spine treatment as a more comprehensive approach. This is part of our Physio Blend for Cervicogenic Dizziness Treatment. Therefore, it can help more than those with just Cervicogenic Dizziness but those too with nautical vertigo.
CERVICOGENIC DIZZINESS COURSES AND CERVICAL VERTIGO COURSES
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the authors (husband–a manual therapist a wife—a vestibular specialist), teach a very unique course combining both the theory and practice of vestibular and manual principles in their 2-day course. Pertinent to this blog post, the entire weekend includes the most up-to-date evidence review from multiple disciplines to diagnose through the “Optimal Sequence Algorithm” and treat through the “Physio Blend”.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for prices and discounts.
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Danielle N. Vaughan, PT, DPT, Vestibular Specialist